Since the beginning of the year, more than 300 surgical interventions have been performed on the basis of the departments of anesthesiology and IT, department of cardiosurgery, endovascular and extracorporeal technologies of NMAPE named after PL Shupyk and SE "Institute of the heart of the Ministry of Healthcare of Ukraine". Among them there are a large number of unique operations with a high surgical and anesthetic risk. One of these operations is complete debranching with subsequent aneurysm endoprosthesis of the thoracic aorta.

According to statistics, 2000 cases of aortic aneurysm are diagnosed annually in the US. The prevalence of this disease is 5-20 cases per million population per year. In pathoanatomical studies of those who died from non-traumatic causes, aortic aneurysm are detected in 1.5% of cases. In the absence of surgical treatment, 3 month mortality is 90% for such a contingent of patients.
Introduction to the clinical practice of aortic endoprosthesis significantly changed the idea of surgical treatment of the pathology of the thoracic aorta. Currently, the hybrid method of surgical correction of diseases of the thoracic aorta is of great interest, which is currently actively being implemented at the Institute of the heart of the Ministry of Healthcare of Ukraine.
Comparable treatment outcomes and fewer complications compared with the traditional method of surgical treatment, make this approach a better choice for the treatment of patients with high surgical risk. Hybrid surgery of the thoracic aorta includes a combination of endoprosthetics and debranching of the branches of the aortic arc.
Debranching is a method of hybrid correction of aortic aneurysms, the essence of which is previous shunting (prosthetics) of the large branches of the aorta with a view to their switching and subsequent implantation of stent grafts in the aneurysmally distended part of aorta. As a result of such an intervention, the risk of ischemic complications and fatalities in comparison with open surgical operations is minimized, due to a decrease in the time of aortic clamping, the time of CPB and the duration of cerebral ischemia and visceral organs.
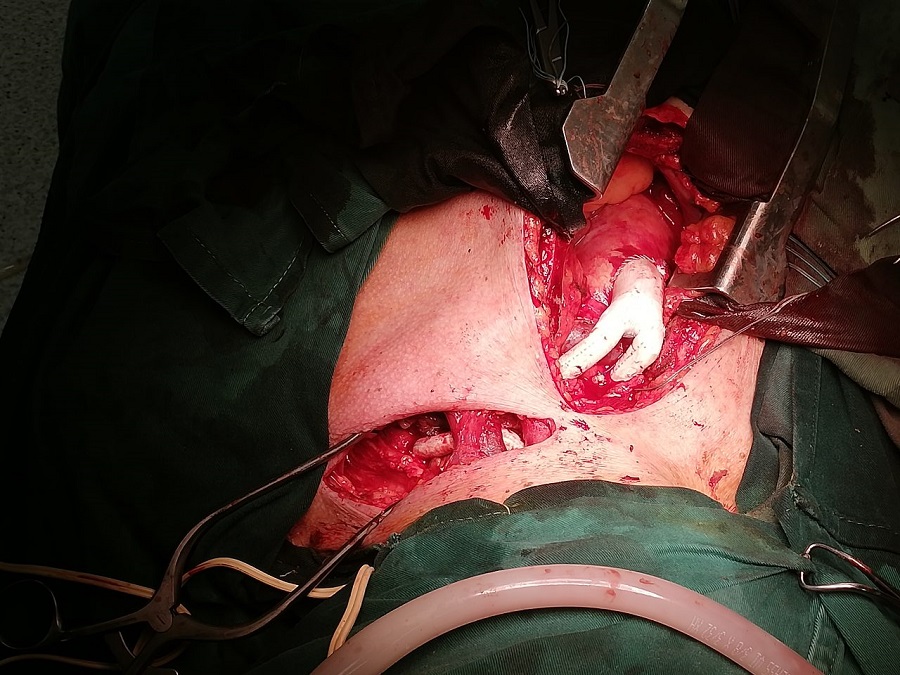
One of such operations was recently performed under the supervision of the head of the Department of Cardiac Surgery, Endovascular and Extracorporeal Technologies of the NMAPE named after PL Shupyk prof. Todurov BM.
The operation involved two surgical and one anesthetic brigade.
The anesthetic provision of this type of surgical interventions required the application of new approaches and methods that are successfully implemented at the department, which involve simultaneous regulation of hemodynamics, cardiac activity and cerebral blood flow.
The operation lasted about four hours. Transfer to weaning from MV was completed after 3 hours postop. Currently, the patient is preparing for discharging.



